
500 kcal/day
That is the daily calorie intake deficit the insuarance companies want you to document properly
150 minutes/day
That is the weekly activities/walking minutes the insuarance companies want you to document properly
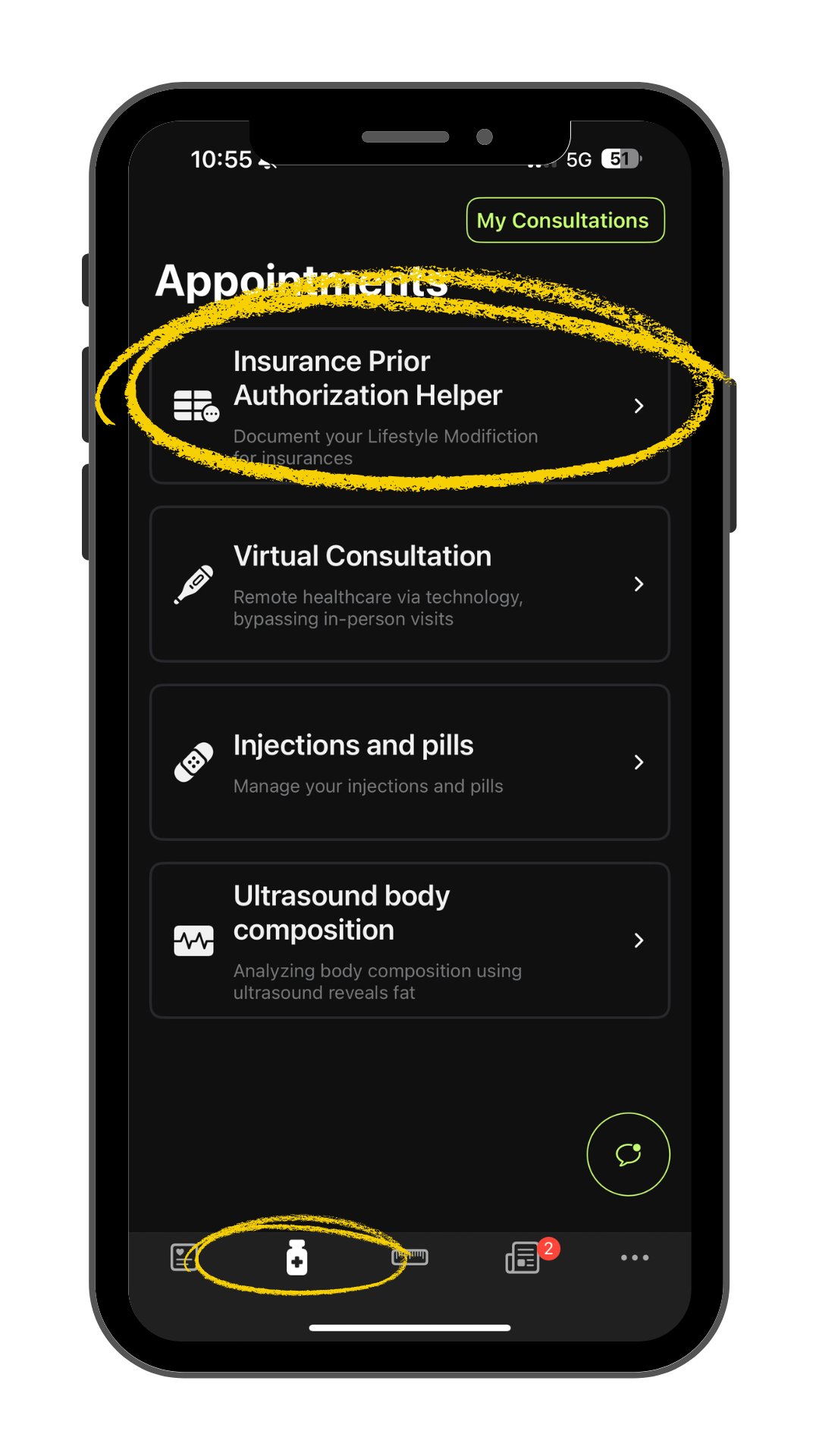
To streamline this process and meet insurance requirements with ease, the Semaglutide App for GLP-1 offers everything you need to properly document your journey.
Quickly track meals and monitor caloric intake to stay consistent with a 500-calorie deficit goal.
Syncs with Apple Health to pull in walking and movement data effortlessly, helping you hit that 150-minute weekly target.
download nowCreates clean, exportable reports you can send directly to your primary care provider or insurance company to support prior authorization requests.
download nowTailored to those pursuing semaglutide/tirzepatide therapy, with reminders, education, and updates relevant to your medication and insurance path
download now
And use the **Semaglutide App** to track, organize, and generate the exact proof insurers need. You’re not just showing your effort—you’re unlocking access to treatment that could change your life.
